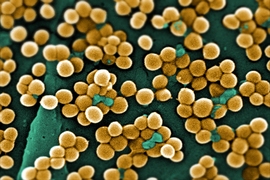
In recent years, new strains of bacteria have emerged that resist even the most powerful antibiotics. Each year, these superbugs, including drug-resistant forms of tuberculosis and staphylococcus, infect more than 2 million people nationwide, and kill at least 23,000. Despite the urgent need for new treatments, scientists have discovered very few new classes of antibiotics in the past decade.
MIT engineers have now turned a powerful new weapon on these superbugs. Using a gene-editing system that can disable any target gene, they have shown that they can selectively kill bacteria carrying harmful genes that confer antibiotic resistance or cause disease.
Led by Timothy Lu, an associate professor of biological engineering and electrical engineering and computer science, the researchers described their findings in the Sept. 21 issue of Nature Biotechnology. Last month, Lu’s lab reported a different approach to combating resistant bacteria by identifying combinations of genes that work together to make bacteria more susceptible to antibiotics.
Lu hopes that both technologies will lead to new drugs to help fight the growing crisis posed by drug-resistant bacteria.
“This is a pretty crucial moment when there are fewer and fewer new antibiotics available, but more and more antibiotic resistance evolving,” he says. “We’ve been interested in finding new ways to combat antibiotic resistance, and these papers offer two different strategies for doing that.”
Cutting out resistance
Most antibiotics work by interfering with crucial functions such as cell division or protein synthesis. However, some bacteria, including the formidable MRSA (methicillin-resistant Staphylococcus aureus) and CRE (carbapenem-resistant Enterobacteriaceae) organisms, have evolved to become virtually untreatable with existing drugs.
In the new Nature Biotechnology study, graduate students Robert Citorik and Mark Mimee worked with Lu to target specific genes that allow bacteria to survive antibiotic treatment. The CRISPR genome-editing system presented the perfect strategy to go after those genes.
CRISPR, originally discovered by biologists studying the bacterial immune system, involves a set of proteins that bacteria use to defend themselves against bacteriophages (viruses that infect bacteria). One of these proteins, a DNA-cutting enzyme called Cas9, binds to short RNA guide strands that target specific sequences, telling Cas9 where to make its cuts.
Lu and colleagues decided to turn bacteria’s own weapons against them. They designed their RNA guide strands to target genes for antibiotic resistance, including the enzyme NDM-1, which allows bacteria to resist a broad range of beta-lactam antibiotics, including carbapenems. The genes encoding NDM-1 and other antibiotic resistance factors are usually carried on plasmids — circular strands of DNA separate from the bacterial genome — making it easier for them to spread through populations.
When the researchers turned the CRISPR system against NDM-1, they were able to specifically kill more than 99 percent of NDM-1-carrying bacteria, while antibiotics to which the bacteria were resistant did not induce any significant killing. They also successfully targeted another antibiotic resistance gene encoding SHV-18, a mutation in the bacterial chromosome providing resistance to quinolone antibiotics, and a virulence factor in enterohemorrhagic E. coli.
In addition, the researchers showed that the CRISPR system could be used to selectively remove specific bacteria from diverse bacterial communities based on their genetic signatures, thus opening up the potential for “microbiome editing” beyond antimicrobial applications.
To get the CRISPR components into bacteria, the researchers created two delivery vehicles — engineered bacteria that carry CRISPR genes on plasmids, and bacteriophage particles that bind to the bacteria and inject the genes. Both of these carriers successfully spread the CRISPR genes through the population of drug-resistant bacteria. Delivery of the CRISPR system into waxworm larvae infected with a harmful form of E. coli resulted in increased survival of the larvae.
The researchers are now testing this approach in mice, and they envision that eventually the technology could be adapted to deliver the CRISPR components to treat infections or remove other unwanted bacteria in human patients.
“This work represents a very interesting genetic method for killing antibiotic-resistant bacteria in a directed fashion, which in principle could help to combat the spread of antibiotic resistance fueled by excessive broad-spectrum treatment,” says Ahmad Khalil, an assistant professor of biomedical engineering at Boston University who was not part of the research team.
High-speed genetic screens
Another tool Lu has developed to fight antibiotic resistance is a technology called CombiGEM. This system, described in the Proceedings of the National Academy of Sciences the week of Aug. 11, allows scientists to rapidly and systematically search for genetic combinations that sensitize bacteria to different antibiotics.
To test the system, Lu and his graduate student, Allen Cheng, created a library of 34,000 pairs of bacterial genes. All of these genes code for transcription factors, which are proteins that control the expression of other genes. Each gene pair is contained on a single piece of DNA that also includes a six-base-pair barcode for each gene. These barcodes allow the researchers to rapidly identify the genes in each pair without having to sequence the entire strand of DNA.
“You can take advantage of really high-throughput sequencing technologies that allow you, in a single shot, to assess millions of genetic combinations simultaneously and pick out the ones that are successful,” Lu says.
The researchers then delivered the gene pairs into drug-resistant bacteria and treated them with different antibiotics. For each antibiotic, they identified gene combinations that enhanced the killing of target bacteria by 10,000- to 1,000,000-fold. The researchers are now investigating how these genes exert their effects.
“This platform allows you to discover the combinations that are really interesting, but it doesn’t necessarily tell you why they work well,” Lu says. “This is a high-throughput technology for uncovering genetic combinations that look really interesting, and then you have to go downstream and figure out the mechanisms.”
Once scientists understand how these genes influence antibiotic resistance, they could try to design new drugs that mimic the effects, Lu says. It is also possible that the genes themselves could be used as a treatment, if researchers can find a safe and effective way to deliver them.
CombiGEM also enables the generation of combinations of three or four genes in a more powerful way than previously existing methods. “We’re excited about the application of CombiGEM to probe complex multifactorial phenotypes, such as stem cell differentiation, cancer biology, and synthetic circuits,” Lu says.
The research was funded by the National Institutes of Health, the Defense Threat Reduction Agency, the U.S. Army Research Laboratory, the U.S. Army Research Office, the Office of Naval Research, and the Ellison Medical Foundation.