Individuals with mild cognitive impairment, especially of the “amnestic subtype” (aMCI), are at increased risk for dementia due to Alzheimer’s disease relative to cognitively healthy older adults. Now, a study co-authored by researchers from MIT, Cornell University, and Massachusetts General Hospital has identified a key deficit in people with aMCI, which relates to producing complex language.
This deficit is independent of the memory deficit that characterizes this group and may provide an additional “cognitive biomarker” to aid in early detection — the time when treatments, as they continue to be developed, are likely to be most effective.
The researchers found that while individuals with aMCI could appreciate the basic structure of sentences (syntax) and their meaning (semantics), they struggled with processing certain ambiguous sentences in which pronouns alluded to people not referenced in the sentences themselves.
“These results are among the first to deal with complex syntax and really get at the abstract computation that’s involved in processing these linguistic structures,” says MIT linguistics scholar Suzanne Flynn, co-author of a paper detailing the results.
The focus on subtleties in language processing, in relation to aMCI and its potential transition to dementia such as Alzheimer’s disease is novel, the researchers say.
“Previous research has looked most often at single words and vocabulary,” says co-author Barbara Lust, a professor emerita at Cornell University. “We looked at a more complex level of language knowledge. When we process a sentence, we have to both grasp its syntax and construct a meaning. We found a breakdown at that higher level where you’re integrating form and meaning.”
The paper, “Disintegration at the syntax-semantics interface in prodromal Alzheimer’s disease: New evidence from complex sentence anaphora in amnestic Mild Cognitive Impairment (aMCI),” appears in the Journal of Neurolinguistics.
The paper’s authors are Flynn, a professor in MIT’s Department of Linguistics and Philosophy; Lust, a professor emerita in the Department of Psychology at Cornell and a visiting scholar and research affiliate in the MIT Department of Linguistics and Philosophy; Janet Cohen Sherman, an associate professor of psychology in the Department of Psychiatry at Massachusetts General Hospital and director of the MGH Psychology Assessment Center; and, posthumously, the scholars James Gair and Charles Henderson of Cornell University.
Anaphora and ambiguity
To conduct the study, the scholars ran experiments comparing the cognitive performance of aMCI patients to cognitively healthy individuals in separate younger and older control groups. The research involved 61 aMCI patients of Massachusetts General Hospital, with control group research conducted at Cornell and MIT.
The study pinpointed how well people process and reproduce sentences involving “anaphora.” In linguistics terms, this generally refers to the relation between a word and another form in the sentence, such the use of “his” in the sentence, “The electrician repaired his equipment.” (The term “anaphora” has another related use in the field of rhetoric, involving the repetition of terms.)
In the study, the researchers ran a variety of sentence constructions past aMCI patients and the control groups. For instance, in the sentence, “The electrician fixed the light switch when he visited the tenant,” it is not actually clear if “he” refers to the electrician, or somebody else entirely. The “he” could be a family member, friend, or landlord, among other possibilities.
On the other hand, in the sentence, “He visited the tenant when the electrician repaired the light switch,” “he” and the electrician cannot be the same person. Alternately, in the sentence, “The babysitter emptied the bottle and prepared the formula,” there is no reference at all to a person beyond the sentence.
Ultimately, aMCI patients performed significantly worse than the control groups when producing sentences with “anaphoric coreference,” the ones with ambiguity about the identity of the person referred to via a pronoun.
“It’s not that aMCI patients have lost the ability to process syntax or put complex sentences together, or lost words; it’s that they’re showing a deficit when the mind has to figure out whether to stay in the sentence or go outside it, to figure out who we’re talking about,” Lust explains. “When they didn’t have to go outside the sentence for context, sentence production was preserved in the individuals with aMCI whom we studied.”
Flynn notes: “This adds to our understanding of the deterioration that occurs in early stages of the dementia process. Deficits extend beyond memory loss. While the participants we studied have memory deficits, their memory difficulties do not explain our language findings, as evidenced by a lack of correlation in their performance on the language task and their performances on measures of memory. This suggests that in addition to the memory difficulties that individuals with aMCI experience, they are also struggling with this central aspect of language.”
Looking for a path to treatment
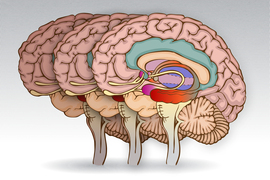
The current paper is part of an ongoing series of studies that Flynn, Lust, Sherman, and their colleagues have performed. The findings have implications for potentially steering neuroscience studies toward regions of the brain that process language, when investigating MCI and other forms of dementia, such as primary progressive aphasia. The study may also help inform linguistics theory concerning various forms of anaphora.
Looking ahead, the scholars say they would like to increase the size of the studies as part of an effort to continue to define how it is that diseases progress and how language may be a predictor of that.
“Our data is a small population but very richly theoretically guided,” Lust says. “You need hypotheses that are linguistically informed to make advances in neurolinguistics. There’s so much interest in the years before Alzheimer’s disease is diagnosed, to see if it can be caught and its progression stopped.”
As Flynn adds, “The more precise we can become about the neuronal locus of deterioration, that’s going to make a big difference in terms of developing treatment.”
Support for the research was provided by the Cornell University Podell Award, Shamitha Somashekar and Apple Corporation, Federal Formula Funds, Brad Hyman at Massachusetts General Hospital, the Cornell Bronfenbrenner Center for Life Course Development, the Cornell Institute for Translational Research on Aging, the Cornell Institute for Social Science Research, and the Cornell Cognitive Science Program.